HBOT & Dental

Conditions Benefitted
- Osteomyelitis
- Osteoradionecrosis
- Non healing wounds
- Non healing infection
- Post oral surgery healing
How will YOUR patient benefit?
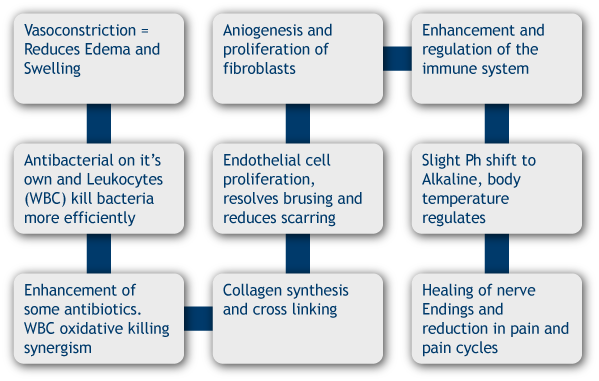
Dental surgeons utilize HBOT because it:- Significantly shortens the inflammation process
- Growth of new blood vessels (Angiogenesis)
- Increases oxygen perfusion area around wounds
- Increases new capillary growth
- Increases production and improves the action of osteoblasts and osteoclasts
- Helps prevent infection
- Enhances the ability of Leukocytes to remove bacteria and debris
- Potentiates the use of antibiotics and helps kill bacteria
HBOT is used commonly before and/or after surgery
HBOT can help to heal bone disorders by stimulating both the osteoclasts and the osteoblasts. This helps and leads to the re-absorption of dead bone and the creation of new bone. In addition, HBOT stimulates the production of new blood vessels, so that the growing bone receives a steady supply of nutrients, including oxygen. This blood vessel network does two other things: it helps support the function of the osteoclasts, and brings infection fighting white blood cells to the area. Nerve repairing and quicker healing are also positive side effects many notice when undergoing HBOT. A good three-part treatment for bone infections includes the use of antibiotics, surgery to remove the dead bone, and HBOT as a supporting or adjunct treatment. Many dental surgeons are using HBOT before and after surgery.Do you have a patient with Osteomyelitis?
Although Antibiotics will help kill microorganisms in the nonossified tissues around the focus of infection and surgery will remove the macroscopic portions of dead, infected bone, HBO improves host responsiveness by making the environments more favorable to WBC oxidative killing, neovascularization, and resorption, of dead, infected bone (reproduced from Strauss 1987, by permission) K.K. Jain, The Textbook of Hyperbaric Medicine, 5th ed, pg 146Find more information in the Bone-Healing conditions page by clicking the button located beneath these figures.
| Case Studies |
|---|
| 74 patients who needed teeth removed from high-dose radiated mandibles were split into two equal groups. One group underwent tooth removal with standard techniques and antibiotics, while the other group underwent 20 treatments before and 10 treatments after tooth removal hyperbaric oxygen protocol with no antibiotics given at any time. After 6 months, those with exposed, nonhealing mandibles were considered to have osteoradionecrosis.The incidence of osteoradionecrosis was 29.9% in the antibiotic treated group versus 5.4% in the hyperbaric no antibiotic group (p=0.005). In addition, 8 of the 11 affected antibiotic patients required jaw resection and were given HBOT for resolution. Of the 2 patients from the HBOT group who developed osteoradionecrosis, neither required jaw resection, indicating a less severe form of necrosis. The 20/10 protocol has since become the standard treatment protocol for single and multiple tooth removals, as well as for surgery in any radiated tissue. (1985, Marx et al.) |
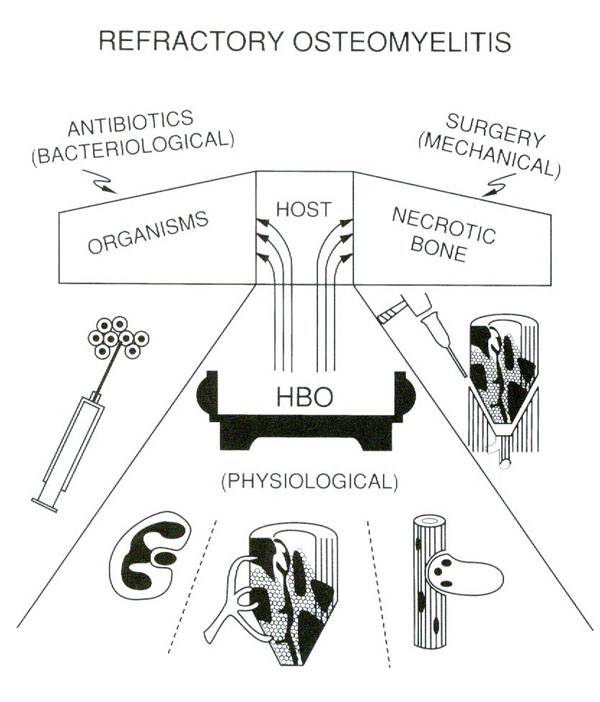 "Figure 13.4" Hyperbaric textbook, pg 146
"Figure 13.4" Hyperbaric textbook, pg 146
Click on the link below to see what conditions related to your medical field are treatable with Hyperbarics. View Conditions Contact